Another Hidden Cause of PCOS Identified? (Gut Dysbiosis)
Most people think that polycystic ovarian syndrome is a situation where your hormones are all messed up. No one disputes that your hormones are messed up. But do you ever wonder how they got that way in the first place?
Free PCOS Newsletter
Many researchers now think the PCOS process started while you were under development in your mother's womb. But that's not what I want to talk about in this article. Let's talk about something that may be causing you problems right now.
One of the most striking features about polycystic ovary syndrome is that there is almost always some degree of chronic inflammation. In other words, your immune system is stirred up. When you immune is stirred up and there is inflammation, all of your body processes become increasingly dysfunctional. That includes your hormones.
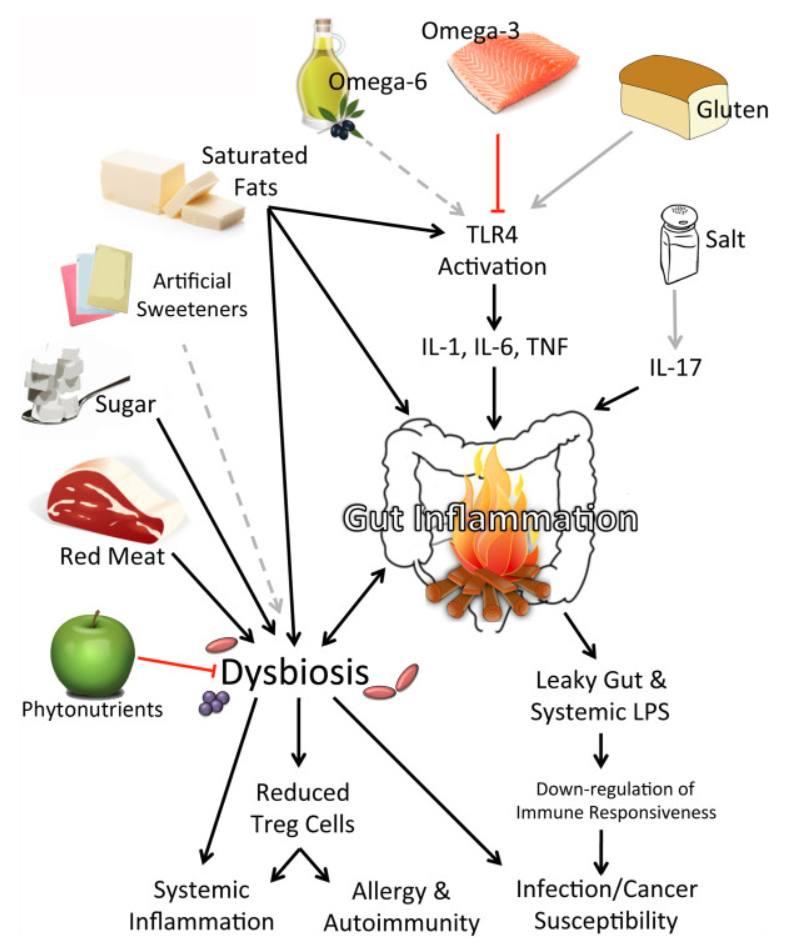
So what might be causing this immune activation and inflammation? Well, you need not look any further than your GI tract. According to a new research paper from Australia, pathogenic bacteria in your gut may cause polycystic ovary syndrome to develop.
Are Unfriendly Intestinal Bacteria PCOS Culprits?
The researchers said they suspect that unfriendly bacteria in the intestines create inflammatory molecules that leak through the barrier between the gut and the bloodstream. These inflammatory materials cause the immune system to react and inflammation is the result.
An activated immune system interferes with insulin receptor function. This prevents insulin from doing its job. And thus a condition called "insulin resistance" is created.
Insulin resistance is widely regarded as the #1 cause of PCOS.
The researchers said that this process can explain menstrual irregularity, polycystic ovaries, and the high level of male hormones that cause acne and hirsutism.
I've looked at some other research. There's no question in my mind that an imbalance of friendly vs. unfriendly bacteria in your gut is one of the main reasons why you have so many symptoms. This imbalance is called "gut dysbiosis".
Maybe some of you were not aware there were any bacteria or other bugs living in your intestines. The fact is that at least 160 different species of bacteria are living in your gut right now. There are ten times more bacteria in your gut than cells in your body. There are millions of them!
The problem is that some of these bacteria are beneficial while others are not. Some are quite harmful. That is, some are wearing white hats (the good guys) and some are wearing black hats (the bad guys).
Your job is to encourage the good guys and discourage the bad guys. If you support the good guys, they will help you get rid of the bad guys.
How To Solve the Problem
Here's how to get started.
1) Change your diet. This is by far your most important step. Medical research has shown that your diet has a profound effect on the bacteria in your gut. You can start off by reducing consumption of saturated fat and greatly increasing the fiber content in your diet (more veggies!!). If you're looking for a diet that supports beneficial bacterial and reduction of symptoms, take a look at our PCOS diet e-book.
2) Don't take antibiotics unless ordered to do so by your doctor. They kill the good guys as well as the bad guys in your gut. When this happens, you can repopulate some of the bacteria by taking a probiotic supplement. A probiotic is a supplement containing several varieties of bacteria.
3) It would be advisable to take a probiotic supplement so long as you have PCOS. Whatever probiotic formula you take, it should contain a variety of organisms. Look at the label. Yogurt and kefir have bacteria, but the amount and variety is insufficient for our purposes.
4) Omega-3 fish oil concentrate has been shown to reduce gut dysbiosis and chronic inflammation, according to research from Harvard Medical School.
Don't underestimate the importance of this article. What's going on in your gut will largely determine how successful you are in getting polycystic ovary syndrome under control.
Source: Tremellen K et al, Dysbiosis of Gut Microbiota (DOGMA)--a novel theory for the development of Polycystic Ovarian Syndrome. Med Hypotheses. 2012 Jul;79(1):104-12.
Kaliannan K et al. A host-microbiome interaction mediates the opposing effects of omega-6 and omega-3 fatty acids on metabolic endotoxemia. Sci Rep. 2015 Jun 11;5:11276.
Return to
Main PCOS Page
Get Answers to your Questions about
- Fertility
- Weight Control
- Hair Loss
- Stress
- Unwanted Hair
- Acne...and more!
FREE PCOS Report
and Newsletter
Your email is safe with us. We respect your privacy, and you may unsubscribe at any time.
Recent Articles
-
PCOS Long Journey to The Happy End
Apr 30, 18 07:24 PM
Hi Girls, Maybe my story will have one day a good end but I am not there yet. Until I was 31 years old I lived my dream, having lovely husband, good -
PCOS and Miscarriage
Apr 17, 18 04:03 PM
Proper diet and natural supplements can help the body maintain a pregnancy through successful delivery.
-
How to Deal with PCOS and Stress
Apr 04, 18 04:19 PM
Your body has a natural capacity to heal itself if you provide it with the necessary tools.