What Is PCOS?
"PCOS" is short for "polycystic ovary syndrome" or "polycystic ovarian syndrome". A "syndrome" is a pattern of symptoms that frequently appear together. It's not a specific disease such as cervical cancer.
We have identified at least 30 different signs and symptoms that may indicate you have this disease. You may have only a few symptoms, or more than a dozen of them.
Free PCOS Newsletter
The most common is "polycystic ovaries", which means an excessive number of underdeveloped follicles on your ovaries. However, you can have polycystic ovaries but not have PCOS.
The most distressing aspects of polycystic ovarian syndrome are inability to ovulate and become pregnant, weight gain, hair loss, unwanted facial and body hair growth, and acne.
But this disease has quite a number of serious consequences that are not always so obvious, including liver disease, hypothyroidism, sleep apnea, appetite disorders, depression and anxiety, high blood fats and blood pressure, and impaired lung function.
There are also longer-term consequences that you will definitely want to prevent. The most prominent ones are a much increased risk of developing diabetes, heart disease and some cancers. A less prominent one is possible brain damage.
Perhaps you're hoping that when you reach menopause, your symptoms will simply go away forever. Your symptoms may change, but the underlying health consequences do not suddenly vanish when you reach menopause. Studies have shown that they persist beyond menopause.
So what does this mean?
Your challenge is that PCOS is a systemic, complex disorder that needs to be actively managed by you for the rest of your life. It is not the type of disorder that can be effectively controlled in the long run by short-term measures such as taking birth control pills.
You need to go to a deeper level and develop certain health practices that will help your body to naturally minimize the symptoms and long-term risks of polycystic ovary syndrome.
If you don't get to work on improving your health practices today, you will pay a heavy price later on.
You don't need to let this disorder ruin your life. You can take action to build and protect your health. You can still live the life of your dreams, but you will have to work for it.
A good place to start is by reading The Natural Diet Solution for PCOS and Infertility e-book, which describes health practices designed specifically to help you get the upper hand.
Sources:
Wang ET et al, Polycystic ovary syndrome and risk for long-term diabetes and dyslipidemia, Obstet Gynecol. 2011 Jan;117(1):6-13.
Rizzo M et al, Long-term consequences of polycystic ovary syndrome on cardiovascular risk, Fertil Steril. 2009 Apr;91(4 Suppl):1563-7
PCOS vs. Polycystic Ovaries - How It Works
In each menstrual cycle, follicles grow on the ovaries. Eggs develop within those follicles, one of which will reach maturity faster than the others and be released into the fallopian tubes. This is "ovulation". The remaining follicles will degenerate.
In the case of polycystic ovaries, however, the ovaries are larger than normal, and there are a series of undeveloped follicles that appear in clumps, somewhat like a bunch of grapes. Polycystic ovaries are not especially troublesome and may not even affect your fertility.
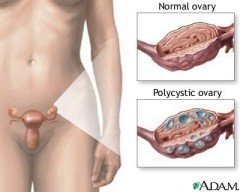
However, when the cysts cause a hormonal imbalance, a pattern of symptoms may develop. This pattern of symptoms is called a syndrome. These symptoms are the difference between suffering from polycystic ovary syndrome and from polycystic ovaries.
So you can have polycystic ovaries without having PCOS. However, nearly all women with PCOS will have polycystic ovaries. Polycystic Ovary Syndrome is the name given to a metabolic condition in which a woman will have polycystic ovaries, along with a certain pattern of other symptoms that reflect imbalances in reproductive and other hormones.
How Is It Diagnosed?
Video below talks about diagnosis:
How it is diagnosed depends on what criteria are used.
The first diagnostic classification was developed in 1990 by the National Institutes of Health. The diagnostic classification required the simultaneous presence of hyperandrogenism (excessive levels of male hormones) and menstrual dysfunction in order to diagnose polycystic ovarian syndrome.
Then in 2003, an expert panel met in Rotterdam and expanded on the previous criteria. They added the presence of PCO (polycystic ovaries) as detected by transvaginal ultrasound. This newer classification broadened the number of women to be diagnosed with PCOS. It included women with irregular periods and polycystic ovaries without hyperandrogenism (abnormally high male hormones), or hyperandrogenism and polycystic ovaries without menstrual dysfunction.
In 2006, the Androgen Excess Society published diagnostic criteria which required the presence of clinical or biochemical hyperandrogenism (abnormally high male hormones), with either polycystic ovaries or menstrual dysfunction to diagnose polycystic ovarian syndrome.
The Rotterdam diagnostic classification is the one that is most commonly used.
Related Articles
- What Is Polycystic Ovary Syndrome?
- Is It Becoming an Epidemic?
- Symptoms You Need to Know About
- What Are the Causes?
- Treatment Information
- Your Family Is at Risk
- Young Girls at Risk
- How to Solve the Puzzle of this Disorder
- Is It More than One Disease?
- Confused? See this Plan to Get a Fresh Start
- New "Gold Standard" for Managing this Disorder
Get Answers to your Questions about
- Fertility
- Weight Control
- Hair Loss
- Stress
- Unwanted Hair
- Acne...and more!
FREE PCOS Report
and Newsletter
Your email is safe with us. We respect your privacy, and you may unsubscribe at any time.
Recent Articles
-
PCOS Long Journey to The Happy End
Apr 30, 18 07:24 PM
Hi Girls, Maybe my story will have one day a good end but I am not there yet. Until I was 31 years old I lived my dream, having lovely husband, good -
PCOS and Miscarriage
Apr 17, 18 04:03 PM
Proper diet and natural supplements can help the body maintain a pregnancy through successful delivery.
-
How to Deal with PCOS and Stress
Apr 04, 18 04:19 PM
Your body has a natural capacity to heal itself if you provide it with the necessary tools.